Chronic obstructive pulmonary disease, or COPD, is a condition where airflow to and from the lungs is limited. This is usually caused by the body's inflammatory response to inhaled irritants like cigarette smoke.
COPD is diagnosed by first assessing your symptoms. COPD takes years to develop and symptoms can be easy to miss because of its slow progression.
Symptoms of early COPD include:
- A chronic cough that brings up clear mucus. This usually occurs in smokers in their 40s and 50s. The cough and amount of mucus may be worse in the mornings, but continues throughout the day. Chronic bronchitis is diagnosed when this kind of cough “occurs most days of the week for three months, in at least two consecutive years” [1].
- Shortness of breath occurring during exertion. Sometimes this is confused with “normal ageing” but it is often a sign of early COPD, particularly in people who have smoked for over 20 years.
COPD becomes increasingly more serious as time goes on, especially if you continue to smoke.

Symptoms of progressed COPD include:
- Recurrent infections like pneumonia. Shortness of breath may become so severe during infections that you require hospitalisation.
- Severe weight loss
- Swelling in the legs
- Morning headaches
If you have any of the symptoms of COPD, or even if you just have a history of smoking, your doctor may ask you to do medical tests to check for signs of COPD.
Tests for COPD
COPD, asthma and any other respiratory diseases have similar symptoms and are often misdiagnosed. Your doctor may want to run tests to rule out other possible causes of your symptoms before diagnosing you with COPD. In some cases, you may be asked to take a test before you experience any symptoms, just based on your history of smoking.
Tests for COPD include:
- Chest x-rays look for signs of emphysema, lung infections, and to rule out other conditions including lung cancer and heart failure.
- Pulmonary function tests measure the total amount of air that you can inhale and exhale, and confirm whether gas exchange is occurring in your lungs – this shows whether your lungs are transferring oxygen into your blood. You may be asked to blow into a large tube connected to a machine that measures how much air your lungs can hold and how fast you can exhale. This test is called spirometry, and it can detect COPD before you even have any symptoms.
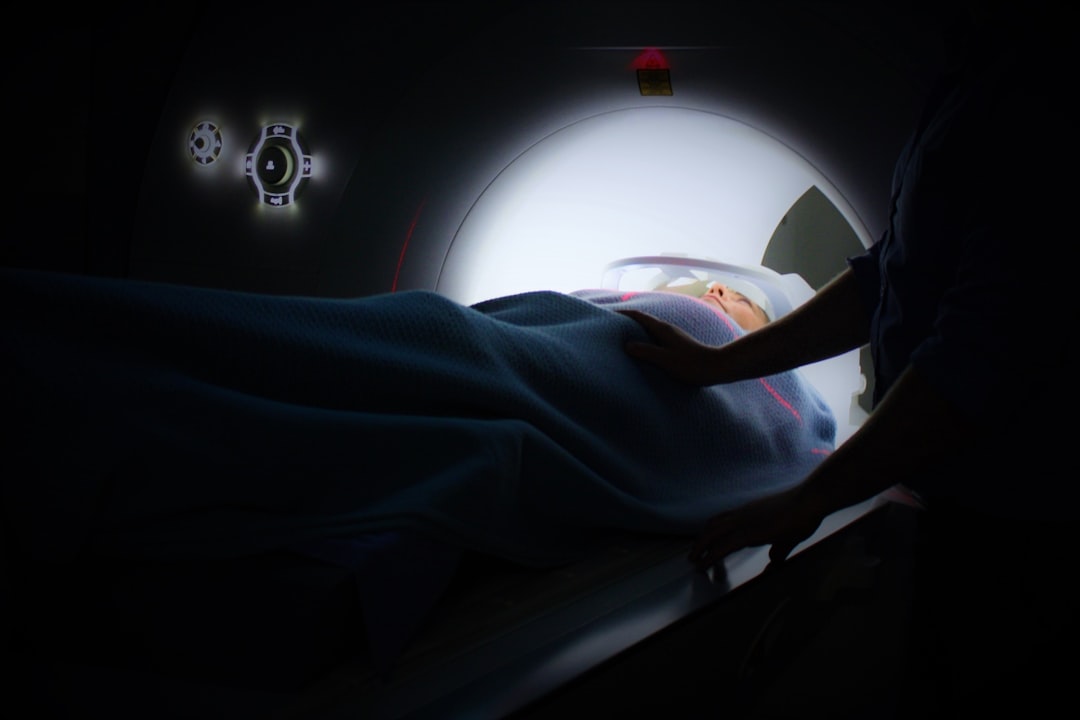
- CT scans can show signs of emphysema. They are also used to rule out lung cancer or to see if you could be a candidate for surgery.
- Electrocardiograms (ECG) can rule out the possibility that a heart condition is causing your symptoms.
- Arterial blood gas is a blood test that measures how well your lungs are bringing in oxygen and releasing carbon dioxide. Blood is usually taken from an artery near the wrist and sent to a lab for analysis.
Your doctor can give you a diagnosis of COPD based on your symptoms, age, how long you've been smoking, and the results of any diagnostic tests. If you are told that you have COPD, don't worry – it's not the end of the world. There are effective treatments for all stages of the disease.
Treatments for COPD
Stop Smoking Right Now
This is non-negotiable. The only way to prevent COPD from getting worse is to stop smoking and avoid exposure to second-hand cigarette smoke. Sure, this kind of pressure to quit smoking doesn't make it any easier to do so, but there is more help and resources available than ever before. Talk to your doctor about support groups, how to handle relapses, and nicotine replacement therapies like patches and gums. You can do it!
Therapies & Medications for COPD
Beyond quitting smoking, there is no “cure” for COPD but medications can help to manage symptoms and complications.
- Oxygen therapy is the only intervention proven to extend life in advanced COPD [2]. It is like an oxygen supplement – when there isn't enough oxygen in your blood, you may need to use a device to boost your levels.
- Bronchodilators are medications that relax the muscles around your airways to relieve coughing and make it easier to breathe. They usually come in an inhaler, and can be short-acting for use before physical activities, or long-acting for daily use.
- Inhaled steroids are used to reduce inflammation in your airways. This creates more space for air to flow through. Inhaled steroids can cause some serious side-effects though, including hoarseness, oral infections, and bruising. Some inhalers combine both steroids and bronchodilators.
- Oral steroids are usually given for a short time during an exacerbation of COPD to stop it from progressing any further. The side-effects of oral steroids can be very serious including diabetes, osteoporosis, cataracts and an increased risk of infections.
- Phosphodiesterase-4 inhibitors also known as PDE4-inhibitors are drugs that block enzymes within immune cells to ultimately reduce inflammation in the airways. They have been shown to reduce the likelihood of COPD exacerbations and can improve lung function, but generally have little impact on quality of life or symptoms. [3]
- Antibiotics are given to treat any respiratory infections that can cause COPD exacerbations. Acute bronchitis and pneumonia can make COPD symptoms much worse, so early treatment with antibiotics can help to prevent an exacerbation or complications of COPD.

Natural Therapies for COPD
- Breathing and relaxation techniques can be used when you're short of breath to open the airways and deliver more oxygen to the lungs. Your doctor may refer you to a respiratory specialist to teach you specific breathing techniques. Doing gentle yoga or getting a massage can relieve stress, and has been shown to immediately improve symptoms of COPD [4].
- Water, humidity and controlled coughing can all help to keep your airways clear. Any accumulation of mucus in the airways can cause breathing difficulties. Water, humidifiers and controlled coughing techniques can keep mucus moving, and nutritents like quercetin, bromelain and N-acetyl-cystine can help to break down the molecules that make mucus “sticky” [5].
- Maintaining a healthy weight can help to manage the symptoms and risks of COPD. While being overweight can make breathing more difficulty, people with COPD who are underweight are more at risk of dying from the disease. In advanced cases, COPD patients burn up to 10 times more calories because of their rapid breathing rate, resulting in muscle loss and poor immune function. To counteract this, supplement your diet with calorie-rich protein shakes, eat more frequently throughout the day, and see a qualified nutritionist for personalised advice.
- Exercise regularly to strengthen your respiratory muscles and endurance. Studies have shown that meditative movement exercises like tai-chi, qigong and yoga can improve lung function and quality of life in COPD [5]. Speak to your doctor about which activities are appropriate for you.
Surgery for COPD
Severe COPD may require surgeries to improve quality life:
- Lung volume reduction is a surgery where a small amount of damaged lung tissue is removed from the upper lungs. This creates more space for the healthier lung tissues to expand into, improving the sensation of breathing and survival rates in COPD.
- Lung transplants are a major surgery and are only a viable option in certain cases. This surgery comes with serious risks including organ rejection. If you have lung transplant surgery for COPD, you will be required to take immunosuppressant medications for the rest of your life.
Chronic obstructive pulmonary disease is diagnosed by a doctor who will consider your history of smoking, your symptoms, and results of medical tests. The frontline treatment for COPD is to quit smoking immediately. Your doctor may speak to you about medications, natural therapies, and possible surgeries that could improve your quality of life, but the foundation for successfully managing COPD is to stop smoking.
References:
[1] Merck Manual Online Database Professional (2018) Chronic Obstructive Pulmonary Disease (COPD). https://www.msdmanuals.com/en-au/professional/pulmonary-disorders/chronic-obstructive-pulmonary-disease-and-related-disorders/chronic-obstructive-pulmonary-disease-copd
[2] McDonald, C. F., et al. (2014) Oxygen therapy for COPD. J Thorac Dis., 6:11, 1632 – 1639. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4255164/
[3] Chong, J., et al. (2017) Phosphodiesterase 4 inhibitors for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. https://www.ncbi.nlm.nih.gov/pubmed/28922692
[4] Yelvar, G. D. Y., et al. (2016) Immediate effect of manual therapy on respiratory functions and inspiratory muscle strength in patients with COPD. Int J Chron Obstruct Pulmon Dis., 11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4920225/
[5] Farazuddin, M., et al. (2018) Quercetin prevents rhinovirus-induced progression of lung disease in mice with COPD phenotype. PloS ONE., 13:7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6033397/
[6] Wu, L., et al. (2018) Effectiveness of meditative movement on COPD: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis., 13, 1239 – 1250. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5909800/